Background
Hereditary hemorrhagic telangiectasia (HHT) is the second most common inherited bleeding disorder (1 in 5000 people) behind von Willebrand disease (VWD) and has no FDA- or EMA-approved therapies. HHT causes serious bleeding resulting in severe iron deficiency anemia, major psychosocial complications, and visceral arteriovenous malformations in brain, lung, and liver that can cause life-threatening hemorrhage, stroke, and other morbid complications. While HHT prevalence is equal in men and women, manifestations may be worse in women (as evidenced by a female predominance in HHT clinical trials). Due to the focus on hemophilia (an X-linked disease nearly exclusive to men) in the hemostasis research community, no study has examined the relative morbidity of the most common inherited bleeding disorders in women: HHT and VWD.
Methods
We performed an observational cohort study of women with HHT or VWD cared for at our institutional Comprehensive Hemophilia and Von Willebrand Disease Treatment Center or HHT Center of Excellence. Using an electronic patient data registry, a representative sample of 100 randomly selected women with HHT were age-matched to 100 randomly selected women with VWD for analysis. All data was extracted and confirmed using manual chart review; we quantified and compared bleeding and healthcare utilization outcomes.
Results
Patient Population. The mean (range) age in both groups was 49 (14-87) years. Mean BMI was 27 in both groups, and racial/ethnic breakdown was similar in both groups. Mean follow-up durations were 9.07 years (HHT) and 14.83 years (VWD) per patient. The VWD group included 86 patients with type 1 VWD and 14 with type 2 VWD.
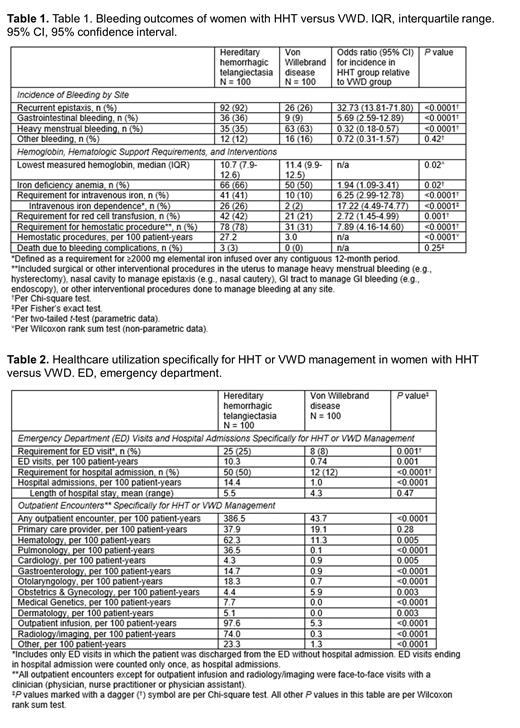
Bleeding Outcomes. Bleeding outcomes are detailed in TABLE 1. In women with HHT compared with VWD, recurrent epistaxis and GI bleeding were more likely (odds ratio [OR] [95% CI] = 32.73 [13.81-71.80], P<0.0001 and 5.69 [2.59-12.89], P<0.0001, respectively), and heavy menstrual bleeding was less likely (OR 0.32 [0.18-0.57], P<0.0001). Iron deficiency anemia was significantly more likely, and lowest hemoglobin significantly lower, in HHT versus VWD. Requirements for IV iron and RBC transfusion were significantly more likely in HHT versus VWD. Women with HHT had 17-fold higher odds of iron infusion dependence and 8-fold higher odds of requiring hemostatic surgical procedures than women with VWD.
Healthcare Utilization for HHT or VWD Management. Healthcare utilization is detailed in TABLE 2. In women with HHT compared with VWD, emergency department (ED) visits and hospital admissions specifically to manage disease complications were significantly more likely (OR [95% CI] = 3.83 [1.67-8.48], P=0.001 and 7.33 [3.57-14.73], P<0.0001, respectively). Rates of ED visitation, admission, and outpatient encounters specifically for HHT or VWD management were significantly higher in women with HHT vs. women with VWD: ED visits, 10.3 per 100 patient-years (pt-yrs) vs. 0.74 per 100 pt-yrs, P=0.001; admissions, 14.4 per 100 pt-yrs vs. 1.0 per 100 pt-yrs, P<0.0001; outpatient encounters, 386.5 per 100 pt-yrs vs. 43.7 per 100 pt-yrs, P<0.0001. Adjusting these rates for the prevalence of HHT (1 in 5000) and VWD (1 in 1000) at the population level, all rates were still higher in the HHT group. Infusion visits, radiology encounters, and nearly all subspecialty provider visit types were much higher in women with HHT ( TABLE 2).
Conclusions
Analyzing matched populations of women at a health system that serves as a tertiary referral center for both diseases, HHT, a historically neglected bleeding disorder, was responsible for much higher morbidity and healthcare utilization in women than VWD, certainly at the individual patient level and possibly at the population level (prevalence-adjusted). Overall incidence of disease complications in each group was consistent with the published literature for both HHT and VWD, supporting the generalizability of our findings. These findings are critically important in achieving gender equity in the hemostasis field, given that both government and industry funding for VWD research is many times greater than for HHT research and such funding for hemophilia research, a disease of men, is at least 10-fold greater than for HHT research. Continued neglect of funding for clinical care and research of HHT within the hemostasis academic community and industry will only sustain and exacerbate gender inequities in hematology.
Disclosures
Al-Samkari:Agios: Consultancy, Research Funding; Sobi: Consultancy, Research Funding; Novartis: Consultancy; Amgen: Research Funding; argenx: Consultancy; Pharmacosmos: Consultancy; Moderna: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal